Abstract
Aims
Most major procedures performed by paediatric surgeons occur with low frequency. Conventional statistical analysis depends on sample size to allow detection of significant differences. It is therefore assumed that variation in operator performance in a low frequency speciality will be impossible to demonstrate. Sequential analysis adopts a different approach to data which is not dependent on probability distributions and sample size; this has been adopted by cardiac surgeons. The analysis may be interpreted graphically, with series which cross limits being designated as out of control. We aimed to analyse leak rates for oesophageal atresia (OA) surgery comparing conventional analysis with statistical process control charts.
Methods
All OA repairs in a regional centre were prospectively recorded. Four consultants had repaired more than 10 OA, and their sequence of repairs and leaks were recorded in chronological order. The leak rate and 95% confidence intervals were calculated for each consultant.
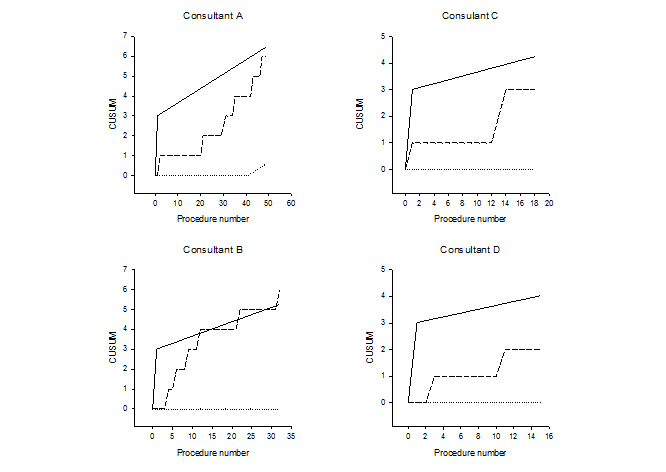
Sequential analysis was performed, setting the target rate for OA leaks at 5%, with a signal rate at 10%, α and β were both set at 10%. CUSUM charts were generated for each consultant.
Results
The leak rate and 95% confidence intervals for these proportions were: Consultant A: 6/49 12% (95%ci 5-24%), Consultant B: 6/32 19% (95%ci 8-35%), Consultant C: 3/19 16% (95%ci 5-37%). Consultant D: 2/16, 12% (3-36%). All leak proportions were within the 95% confidence intervals of each other.
CUSUM charts show that the leak rate for Consultant B was out of control after patient 12 in their series. All other consultant’s series were in control.
Conclusions
Sequential analysis allows discrimination of operator outcomes at low frequency when conventional statistical analysis suggest there is no difference in outcomes. For a low frequency specialty such as paediatric surgery, sequential analysis should be the preferred technique for analysis of outcomes.