Abstract
AIM:
Increased intra-abdominal pressure (IAP) is seen in patients after congenital diaphragmatic hernia (CDH) repair due to reduction of thoracic content into the relatively smaller abdominal cavity. In infants, IAP>10 mmHg is considered Intra-abdominal hypertension (IAH).
This study aimed to determine the incidence of IAH in neonates post CDH repair. We also evaluated the relationship between IAH, and duration of respiratory support and the early return of gastrointestinal function respectively.
Methods: We prospectively recruited all neonates who had CDH repair in our institution from June 2019 to October 2020. Intravesical pressure was used as a proxy for IAP and was measured using a closed system transducer for 5 consecutive days post-surgery. Daily median values were used for analysis. We categorised IAP as <11mmHg (no IAH), 11-15mmHg (IAH) and >15mmHg (severe IAH).
The study was ethically approved (No 201951-7379).
Spearman correlation analysis was used to measure the strength of association between nonparametric data. A value of p < 0.05 was considered statistically significant.
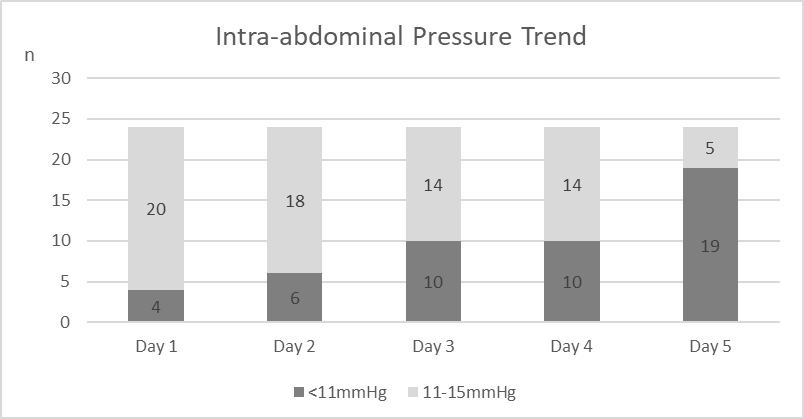
Results: There were 24 neonates included in this study, operated between 1-6 days of life (median age day 4 of life). No patient recorded IAP>15mmHg. The intra-abdominal pressure trend is shown in the figure below:
Figure: Trend of Intra-abdominal Pressure Post Congenital Diaphragmatic Hernia Repair
Those requiring ventilatory support for 4-7 days post repair formed the largest proportion (n=10,41.7%); 7(29.2%) were ventilated <4 days, the remainder >7 days. There was strong correlation between days of IAH and duration of ventilation (p-value<0.001, r=0.704). There was moderate correlation between days of IAH and duration taken for full enteral feeding (p-value 0.005, r=0.704).
Conclusion: IAP measurement is a safe and useful adjunct in post CDH monitoring to detect IAH and in predicting ventilatory support requirements and the time required for feeding establishment.