Abstract
Aim of the Study: Traditionally, pilonidal disease has been treated by wide local excision with or without primary closure. This approach has been associated with a recurrent rate of 5-20% as well as the need for frequent dressing changes. With the growing popularity of less invasive techniques, the purpose of this study was to present our preliminary experience with trephination for pilonidal sinus surgery.
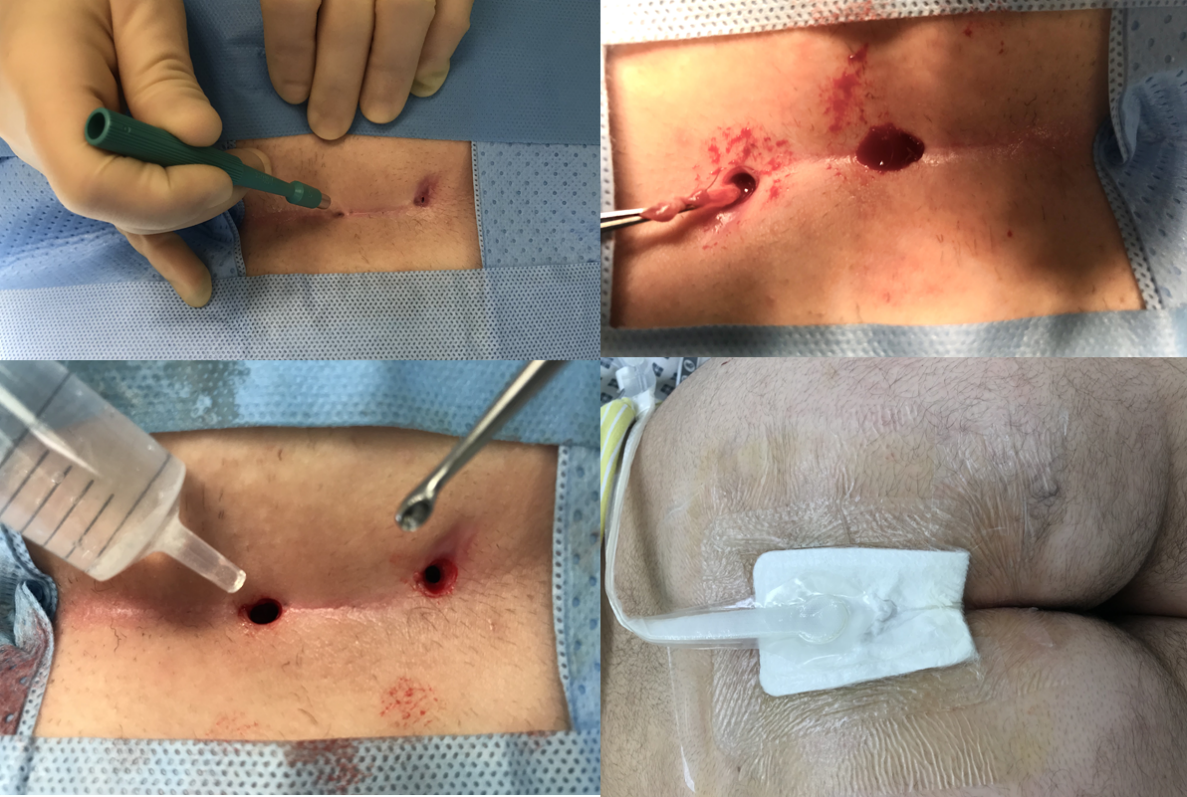
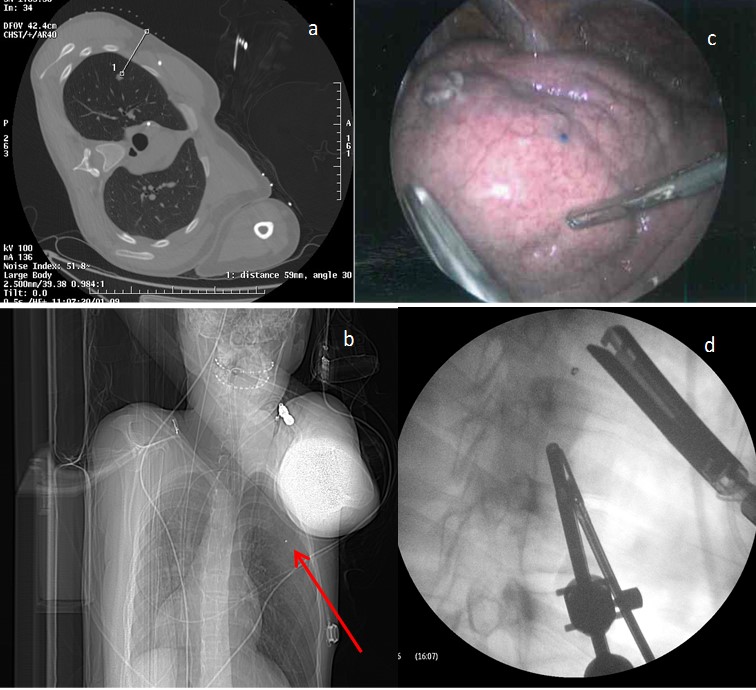
Method: The procedure includes a set of 4 steps :
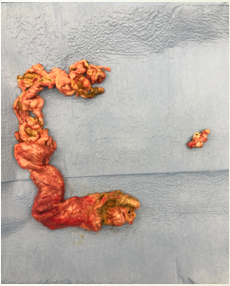
a. Trephination of the sinus exit points using disposable punch biopsy kits (3-8mm)
b. Hair removal from and curettage of the sinus tracts
c. Irrigation with hydrogen peroxide: saline (50:50 mix)
d. Negative suction dressing applied (PICO) at end of procedure (for one week)
Single centre prospective review of pilonidal sinus surgery since April 2019. Patient demographics, operation notes and case notes were reviewed and analysed.
Results: Eight children (4 male) had trephination to their natal cleft, the median age was 16 years. The mean BMI was 26.4 kg/m2. One of the patients had undergone a previous wide local excision (WLE) with primary closure and recurred. The median number of punch biopsies performed was three (range 2-7). Four (50%) children were done as day cases, compared with only 21% (4/19) in our historic cohort (WLE). There was one recurrence, this occurred at the most inferior location on a male who had undergone three punch biopsies at the procedure. The follow up time was a median of 3 months. There were no other complications.
Conclusion: Trephination for pilonidal surgery appears straightforward and feasible following this four step approach. The length of hospital stay is potentially shorter and can more often be day case. Longer term follow up will be required to ensure the recurrence rate is comparable.
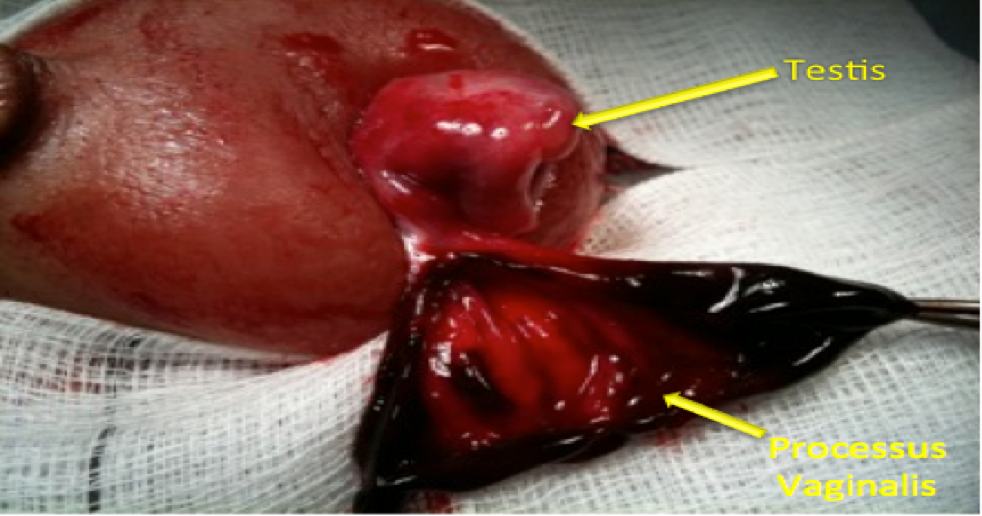
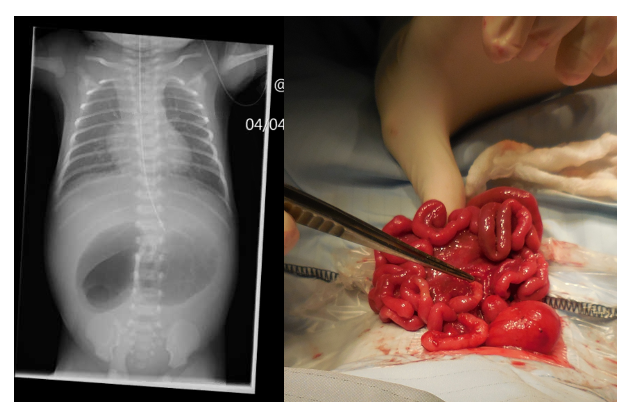
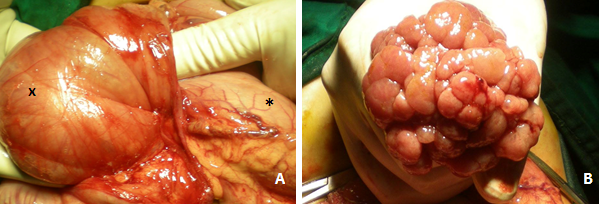
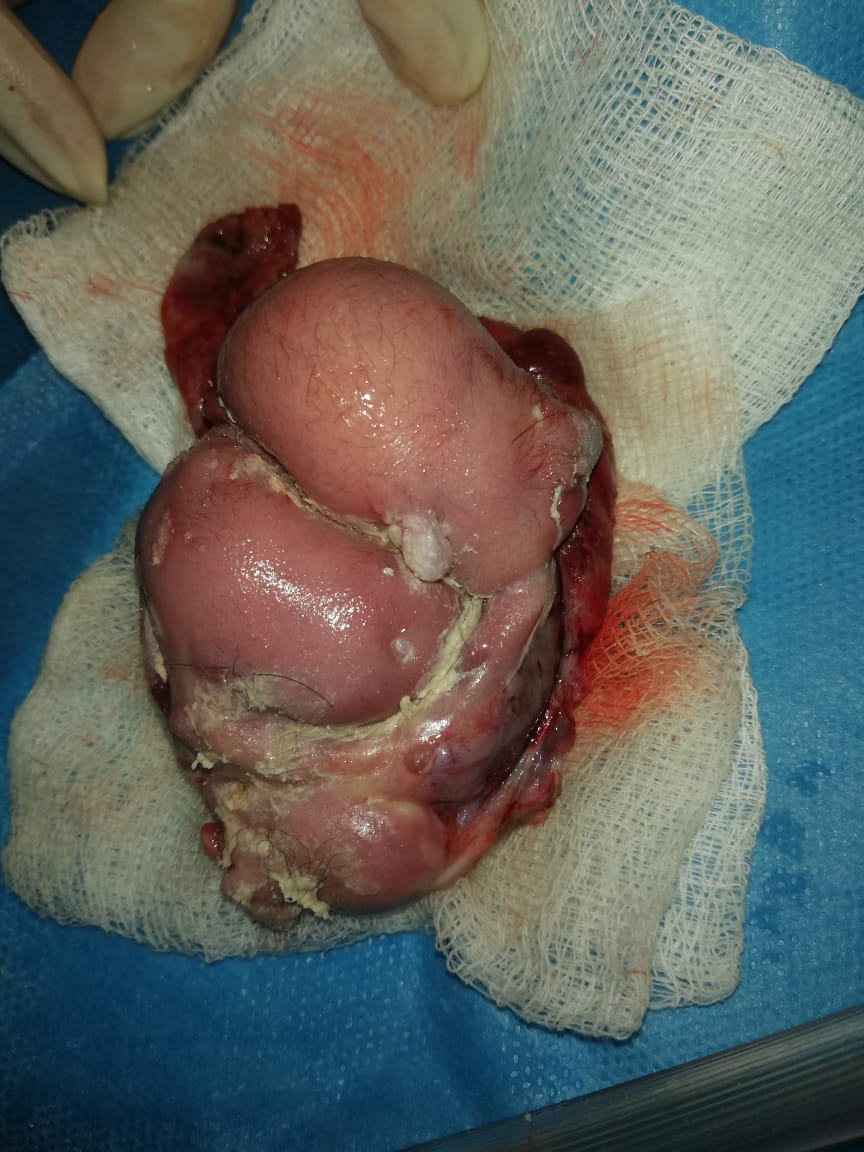
Figure 1: Minimally invasive trephination for pilonidal sinuses in pictures