Primary topic
BACKGROUND
When studying the effect of ankle-foot orthoses (AFOs) on gait, it is important to know their sagittal plane stiffness because it helps explain the effect of AFOs on gait kinematics and kinetics [1]. However, there are no established thresholds for stiffness of non-articulated AFOs designed to be rigid [2]. Hence, if implementing published algorithms for ankle-foot orthosis-footwear combinations (AFO-FCs), it is important to confirm that the AFOs are equally stiff as those of the developer of the AFO-FC algorithms [3].
AIM
To compare the sagittal plane stiffness of AFOs designed to be rigid, made in the USA and following algorithms for AFO-FC designs, to those made and used in the UK by the developer of the AFO-FC algorithms.
METHOD
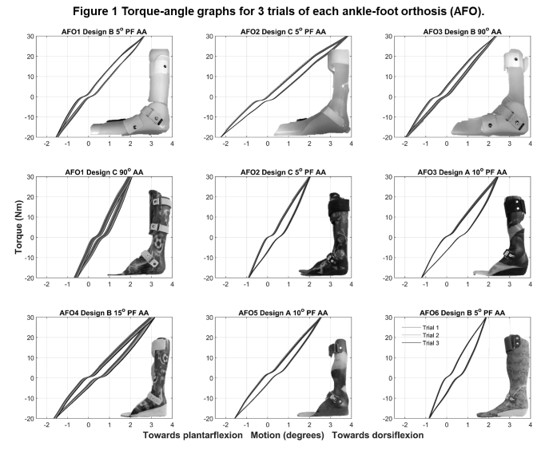
Stiffness of 9 pediatric polypropylene AFOs was tested (UK: 6; USA: 3). A computer controlled motorized device was used [4] in which all AFOs were clamped with the calf shell in a fixed vertical component and the foot section in a rotating plate. Each AFO was tested for 3 trials, loading the foot plate 30 Nm towards dorsiflexion and 20 Nm towards plantarflexion. Torque-angle graphs were plotted and deflection and stiffness compared descriptively across AFOs.
RESULTS
AFO designs tested and torque-angle graphs are shown in Figure 1. Average deflection of AFOs was UK: 3.42±0.83° and USA: 4.81±1.05°. Average stiffness of AFOs was UK: 14.34±3.34 Nm/° and USA: 10.30±1.92 Nm/°.
DISCUSSION AND CONCLUSION
All tested AFOs deflected only a few degrees in either direction (range: 2.59º to 6.02º), providing the first information reported for the stiffness of rigid pediatric non-articulated AFOs. Overall, the UK AFOs were stiffer and deflected less than the USA AFOs. AFO design features such as optimum material for height and weight, ankle rib reinforcements, and trim lines anterior to the malleoli should be carefully considered as they likely influence sagittal plane stiffness and deflection under load.
REFERENCES
1. Totah D, et al. Gait Posture 2019;69:101-11. 2. Ielapi A, et al. Prosthet Orthot Int 2019;43:339-48. 3. Owen E. Prosthet Orthot Int 2010;34:254-69. 4. Gao F, et al. Int Conf Bioinf Biomed Eng. IEEE, 2010;1-4.
ACKNOWLEDGEMENTS
This work was supported by the National Institutes of Health Award #R21HD094823.