Primary topic
BACKGROUND
Socket reaction moment (SRM) has been reported to have a systematic relationship with alignment changes of transtibial prosthetic sockets. Therefore, SRM may be useful to evaluate prosthetic alignment quantitatively. However, the effects of alignment of the prosthetic feet on SRM is still unclear.
AIM
To investigate whether alignment changes of the prosthetic feet (plantarflexion, dorsiflexion, inversion, and eversion) influence SRM systematically in the sagittal and coronal planes.
METHOD
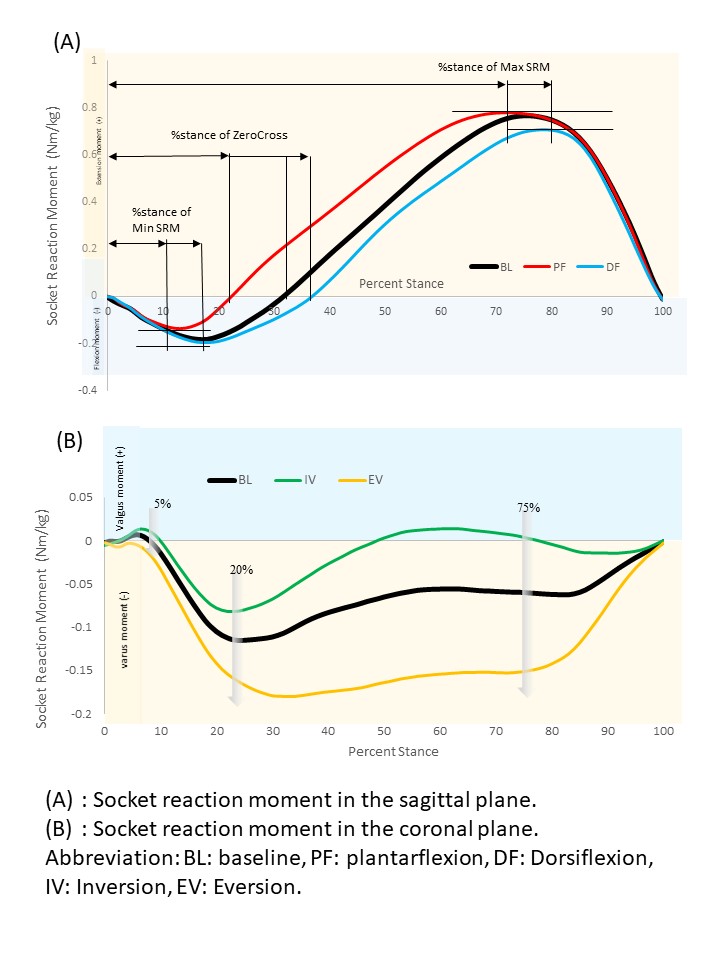
Ten users of transtibial prostheses were recruited in this study. Temporal-spatial parameters (Cadence, walking speed, step time, single support time, and step length) and sagittal and coronal SRM were measured during walking under five alignment conditions (3-degree plantarflexion and dorsiflexion, 6-degree inversion and eversion, and baseline alignment. Minimum and Maximum SRM, % stance (timing) of Minimum and Maximum SRM and zero cross in the sagittal plane, SRM of 5% stance, 20% stance, and 75% stance in the coronal plane were extracted and analyzed. Repeated measures of ANOVA or Friedman tests were carried out for statistical analyses (p < 0.05).
RESULTS
In the coronal plane, SRM of 5% stance, 20% stance, and 75% stance showed significant differences under both inversion and eversion (p=0.018, <0.001, <0.001, respectively). Minimum SRM, % stance of Minimum and Maximum SRM, and zero cross showed significant differences under sagittal alignment changes (plantarflexion/dorsiflexion) (p=0.028, 0.017, <0.001, respectively). There were also significant differences among single support times of the intact side in sagittal alignment changes, step time of the prosthetic side and single support times of the intact side with relation to coronal alignment changes.
DISCUSSION AND CONCLUSION
Our findings suggest that inversion and eversion of transtibial prosthetic feet would affect the magnitude of SRM systematically in the coronal plane, while plantarflexion and dorsiflexion would affect the timing of SRM and Minimum SRM in the sagittal plane. These findings may be beneficial to evaluate and adjust alignment of feet in transtibial prostheses.