Abstract
Objectives
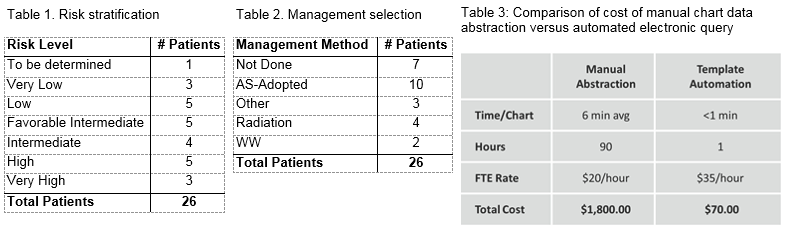
As the U.S. healthcare system shifts from fee-for-service reimbursement to value-based payment paradigms, pay-for-performance (P4P) models have striven to improve the value of healthcare (i.e., improve quality and lower cost). We developed a prostate cancer (PCa) active surveillance (AS) P4P incentive payment model to improve the appropriate adoption and quality of surveillance or watchful waiting (WW) for men with low-risk PCa. Our pilot study develops and tests quality measures, performance thresholds, technology infrastructure and its cost-effectiveness to support the P4P model.
Methods
In collaboration with the national Prostate Cancer Active Surveillance Project (PCASP) consortium, Genesis Healthcare Partners (GHP), developed 4 quality measures: Utilization of an electronic medical record (EMR)-embedded template to capture physician assessed PCa risk and management strategy, Adoption of AS/WW for low-risk PCa, Quality of surveillance with PSA testing, and Quality of surveillance with biopsy procedures. The GHP WizMD® software platform overlays the EMR allowing it to retrieve, organize and report on clinical/pathology data from the EMR-embedded templates. The templates prompt physicians to assess and document the patient’s PCa risk category and management strategy. We undertook a pilot study at a centralized location within GHP.
Results
Compared to manual chart review data abstraction, automated template data abstraction resulted in a 26-fold decrease in cost (n=450 patients x2 visits per year). Template use has been well received. A physician commented: “The template is intuitively easy to use. It takes no more than 1 minute to input the data. While it is an additional step, it is not onerous and appropriate classification and documentation is what we should be doing all the time.”
Conclusions
Value-based payment models, including pay-for-performance, require quality measures that can be assessed with a high degree of fidelity to support a payment-incentive method. Our pilot study shows that detailed PCa data on risk stratification and patient management selection can be efficiently, reliably and cost-effectively retrieved from the EMR using information technology to avoid the need for manual chart review.