Abstract
Introduction
Minimally invasive surgical treatments (MIST) for BPH are an attractive option for men interested in less invasive options, but come with a higher retreatment rate. Salvage holmium laser enucleation of prostate (s-HoLEP) after prior BPH surgery is common however the landscape of MIST treatments has evolved over time.
Methods
A retrospective database of HoLEP procedures from a single center between 6/2006 and 12/2020 was evaluated for patients who had a s-HoLEP.
Results
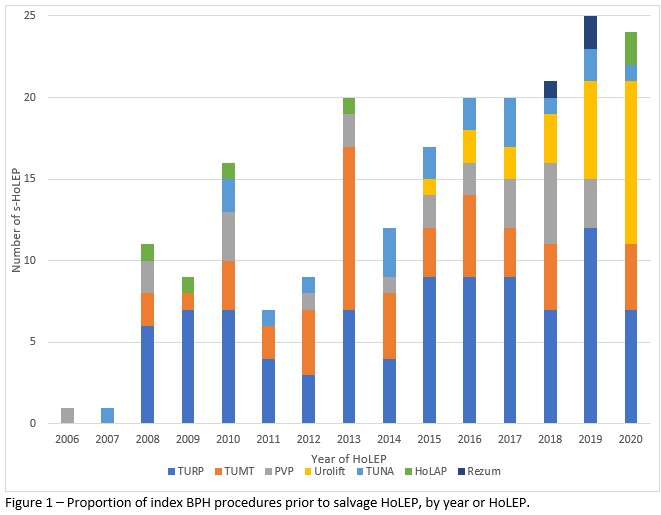
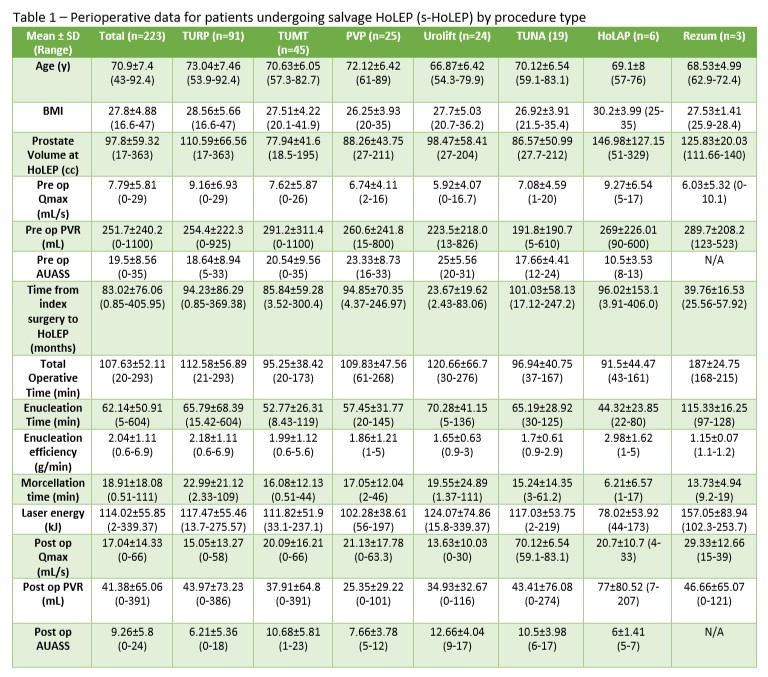
Out of 1960 HoLEPs, 223 (11.3%) were s-HoLEP. BPH procedures that proceeded s-HoLEP included TURP (91, 40.8%), TUMT (45, 20.2%), PVP (25, 11.2%), Urolift (24, 10.8%), TUNA (19, 8.5%), HoLAP (6, 2.7%), and Rezum (3, 1.3%). Only 1 (0.4%) had prior HoLEP. Table 1 outlines patient data by procedure. Mean prostate volume at s-HoLEP was 97.8±59.32 cc (range 17-363) and time from index surgery to s-HoLEP was 83.02±76.06 months (0.85-405.95). Urolift had the shortest interval from index surgery to s-HoLEP (23.67±19.62 months) followed by Rezum (39.76±16.53). Operative times were within expected ranges. Catheter duration was 1.9±1.8 days and POD 1 trial of passage successful in 53.8%. Overall postoperative complication rate was 6.3%. The most common index procedure per year was TURP until 2020 where post-Urolift s-HoLEP became more common (10/24, 42%, Figure 1). The proportion of overall HoLEPs done as a s-HoLEP has ranged from 9-15% and has not changed significantly over time.
Conclusion:
S-HoLEP is a common occurrence in a large HoLEP practice with good functional and safety outcomes. Patients presenting for s-HoLEP have large prostates. The relative proportion of each index procedure is changing with more patients presenting with prior Urolift implants. Surgeons should be aware of this shift and the modifications to surgical technique needed to tackle these cases.