Abstract
Introduction:
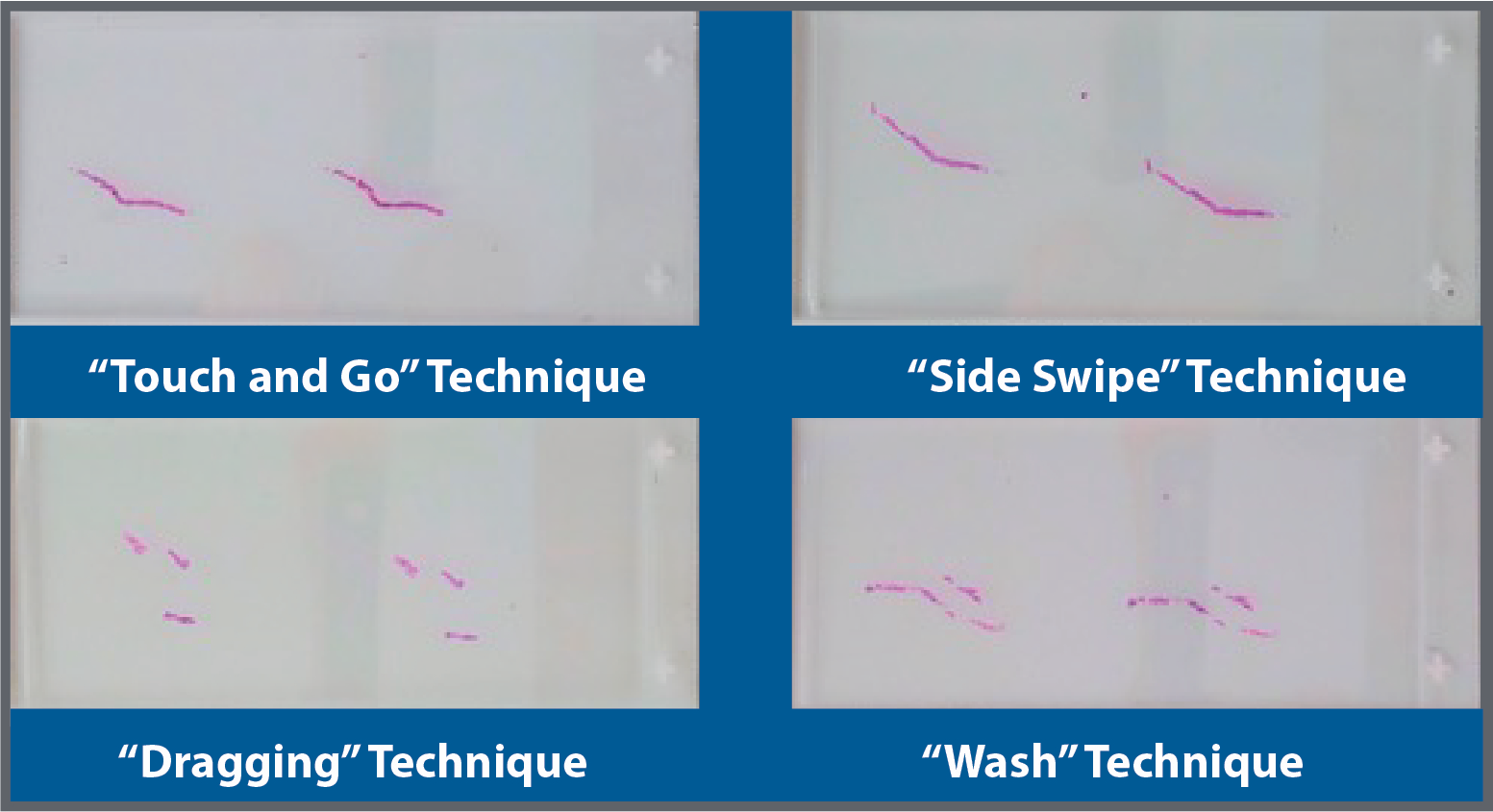
A 69-year-old woman presented to our clinic with bilateral kidney stones. A preoperative computed tomography (CT) scan showed multiple stone fragments in the left distal ureter alongside the stent (Figure 1). The largest stone on the left side measured up to 2 cm. The patient underwent left ureteroscopy with Holmium laser lithotripsy and placement of ureteral stent on April 28, 2021. She did not pass any stone fragments up to 2 weeks after her procedure. With consideration of the COVID-19 pandemic and the patient’s limited physical ability, the patient inspired our novel implementation of hula hooping for facilitating her passage of stone fragments.
Objective:
To evaluate hula hooping for facilitation of passage of kidney stone fragments.
Materials and Methods:
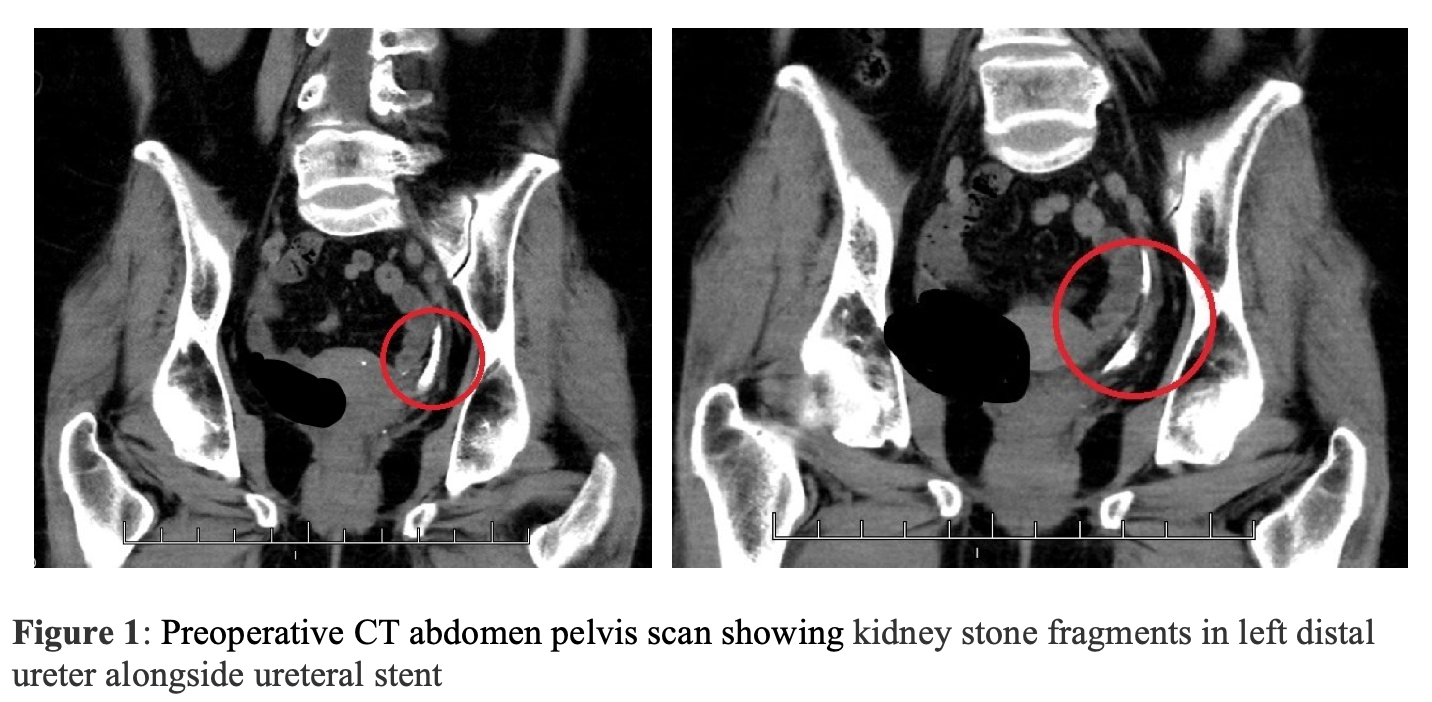
The patient hula hooped for approximately only 5 minutes on May 15, 2021 and passed an impressive amount of stone fragments.
Results:
After hula hooping, the patient passed a multitude of stone fragments and continued to pass fragments afterward (Figure 2).
Conclusion:
Hula hooping is a fun activity that can be added to the urologist armamentarium. Although we provide anecdotal evidence, it presents hula hooping as a viable technique for facilitating passage of kidney stone fragments. Alternatively, mechanistically similar activities, such as Hawaiian belly dancing and twist dancing, may also facilitate passage. As urologists, it is important to be open-minded about fun everyday activities that can also have clinical benefits for patients.
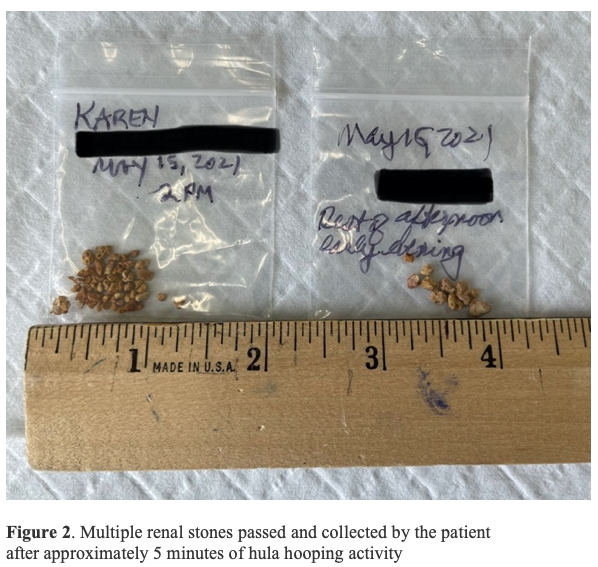


 In this head-to-head comparator study, the novel test needle collected significantly more tissue volume by weight than the SoC needle, 12% in TR and 21% in TP. Additional studies are continuing to assess the impact and utility of this novel biopsy needle design on quantitative and qualitative aspects of histologic processing and diagnosis.
In this head-to-head comparator study, the novel test needle collected significantly more tissue volume by weight than the SoC needle, 12% in TR and 21% in TP. Additional studies are continuing to assess the impact and utility of this novel biopsy needle design on quantitative and qualitative aspects of histologic processing and diagnosis.