Abstract
Introduction and Objective: This observational study evaluated the association between use of active surveillance (AS) and relevant covariates in patients with NCCN favorable intermediate-risk (FIR) prostate cancer (PCa) who received the 17-gene Genomic Prostate Score® (GPSTM) molecular assay.
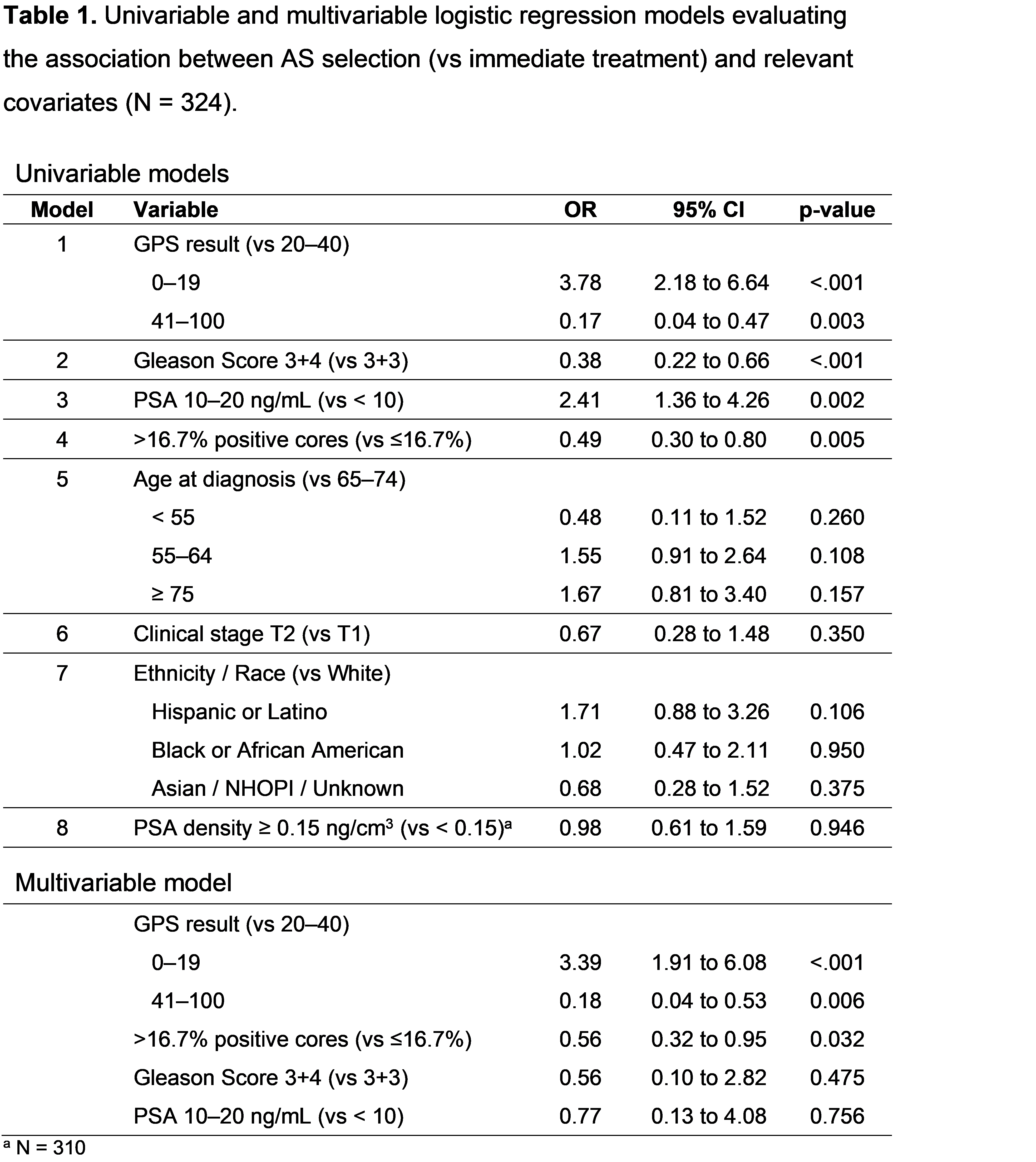
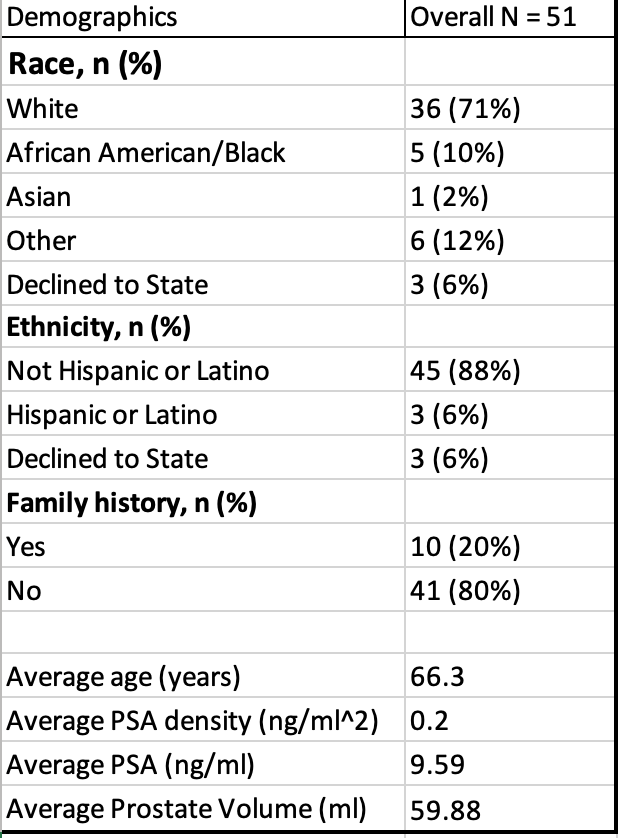
Methods: Contemporary data were collected from both academic and large community urology group practices across the United States. Eligible patients had localized PCa classified as FIR per NCCN guidelines and received a GPS report between May 2017 and April 2019. Higher GPS results (scale: 0-100) are associated with higher risk of adverse outcomes. The proportions of patients selecting active surveillance was calculated with 95% confidence intervals (CI). Uni- and multivariable logistic regression analyses were performed to determine the association between AS selection and relevant covariates.
Results: 324 eligible patients had a median of 12 biopsy cores; 79% had grade group 2 tumors, 19% had PSA 10-20 ng/mL, and 2% were clinical stage T2b. GPS results for 76 patients were <20, 195 were 20-40, and 53 were >40. Overall, 31% (95% CI 26%, 36%) selected AS, with percentages decreasing as GPS results increased. In univariable models, Gleason Score, percent positive cores, PSA, and GPS result were significantly associated with AS selection. In a multivariable model including these variables, percent positive cores and the GPS result remained significantly associated with AS selection (Table 1).
Conclusions: Percent positive cores and the GPS result appear associated with AS use after controlling for relevant clinical variables in NCCN FIR PCa patients.