Abstract
Objectives: Enhanced recovery after surgery (ERAS) protocols have shown to improve the perioperative outcomes in patients undergoing radical cystectomy (RC) for bladder cancer. However, limited data is available regarding the long-term outcomes of these patients. The aim of this study is to evaluate the oncological outcomes in patients who underwent RC with ERAS protocol.
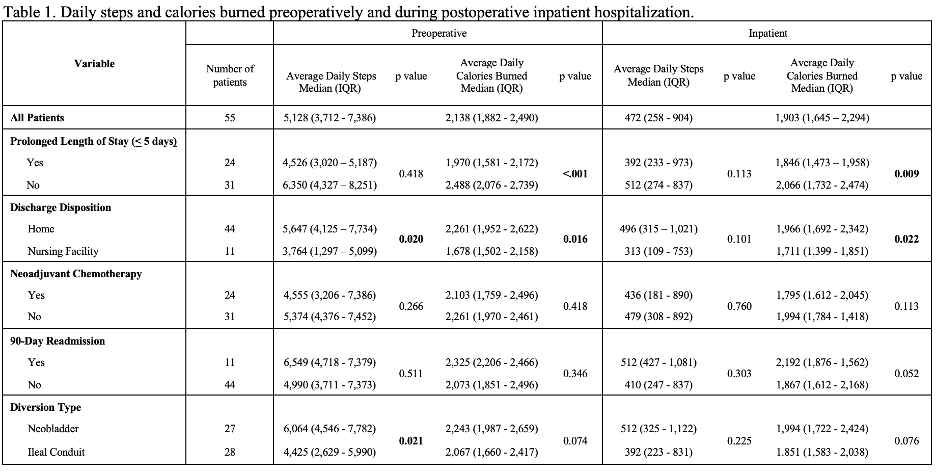
Materials and Methods: Using our IRB-approved bladder cancer database, we reviewed the records of patients who underwent RC for primary urothelial bladder carcinoma with curative intent from January 2003 to December 2019 (ERAS implemented March 2012 on consecutive patients). The primary and secondary outcomes were recurrent-free and overall survival. Multivariable cox regression analysis was performed to evaluate the effect of ERAS as an independent variable on oncological outcomes.
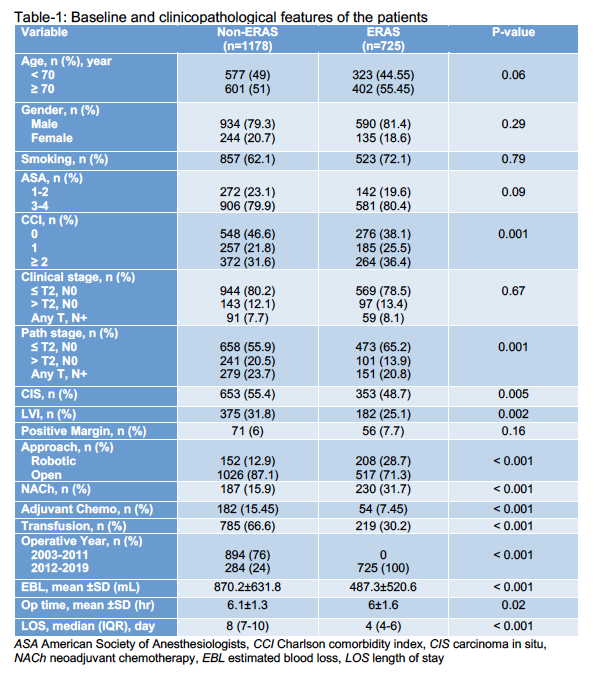
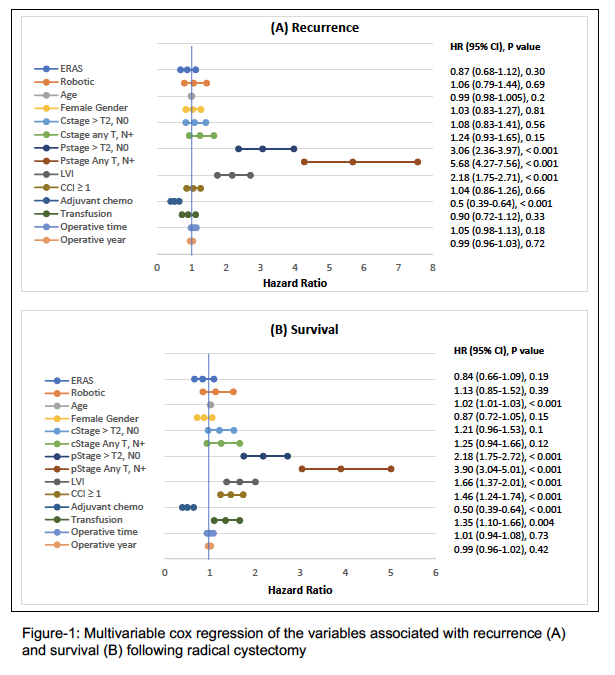
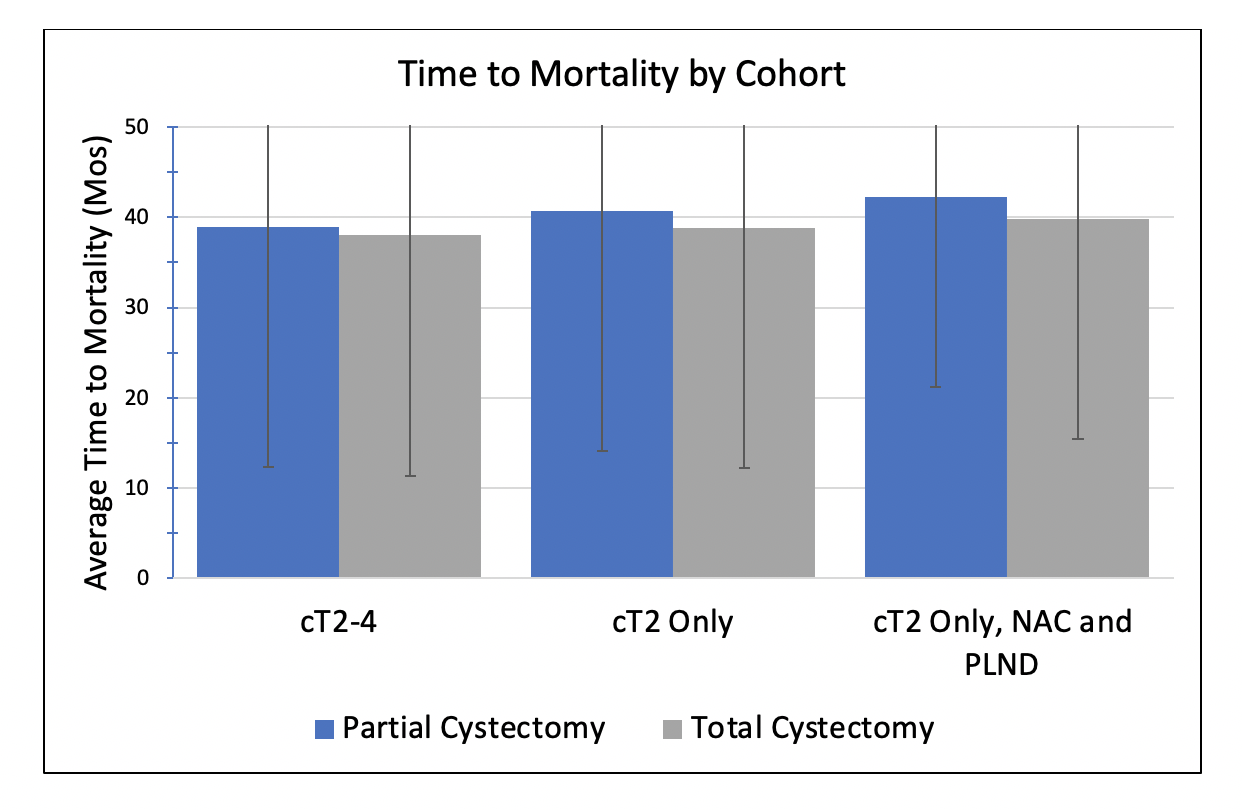
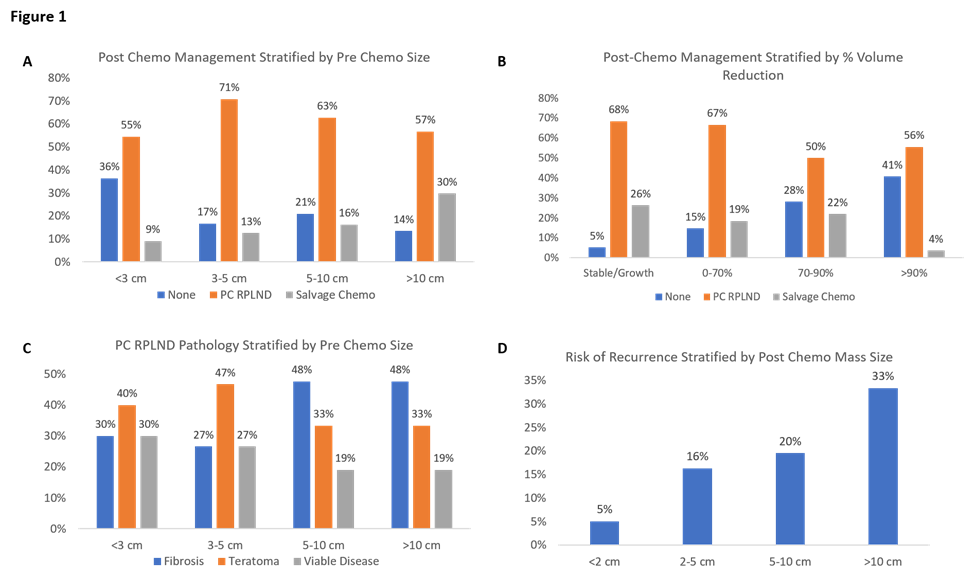
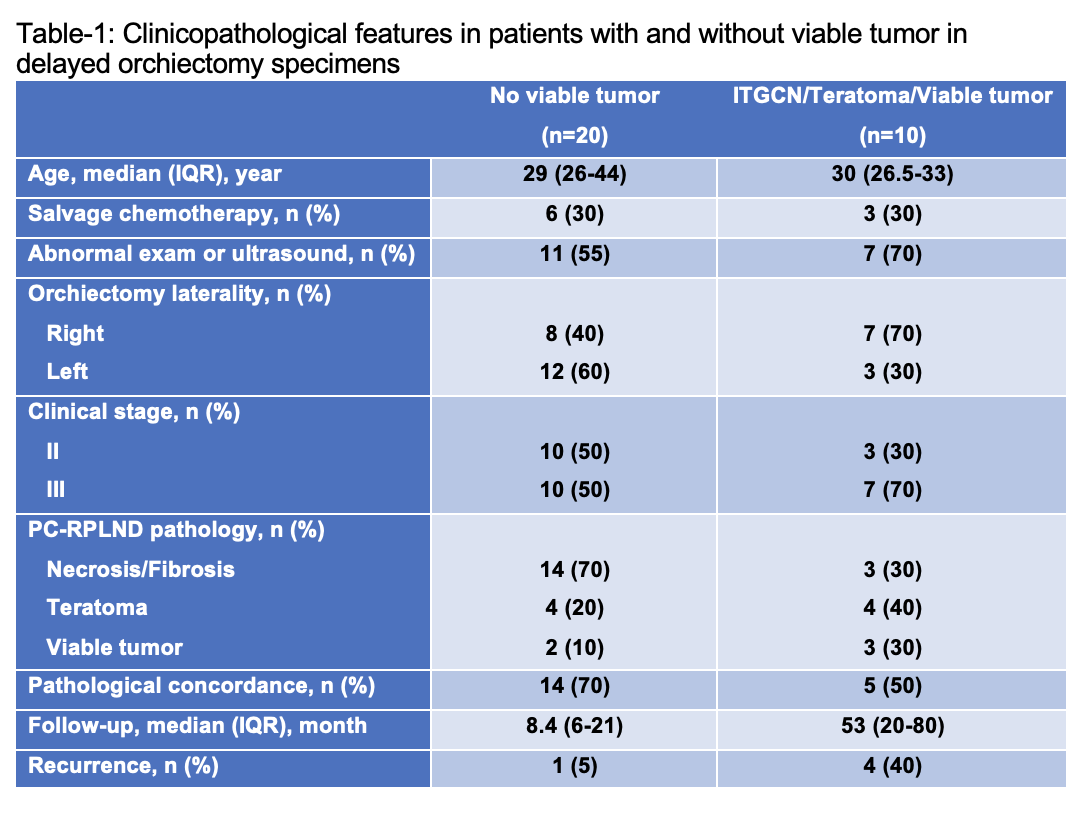
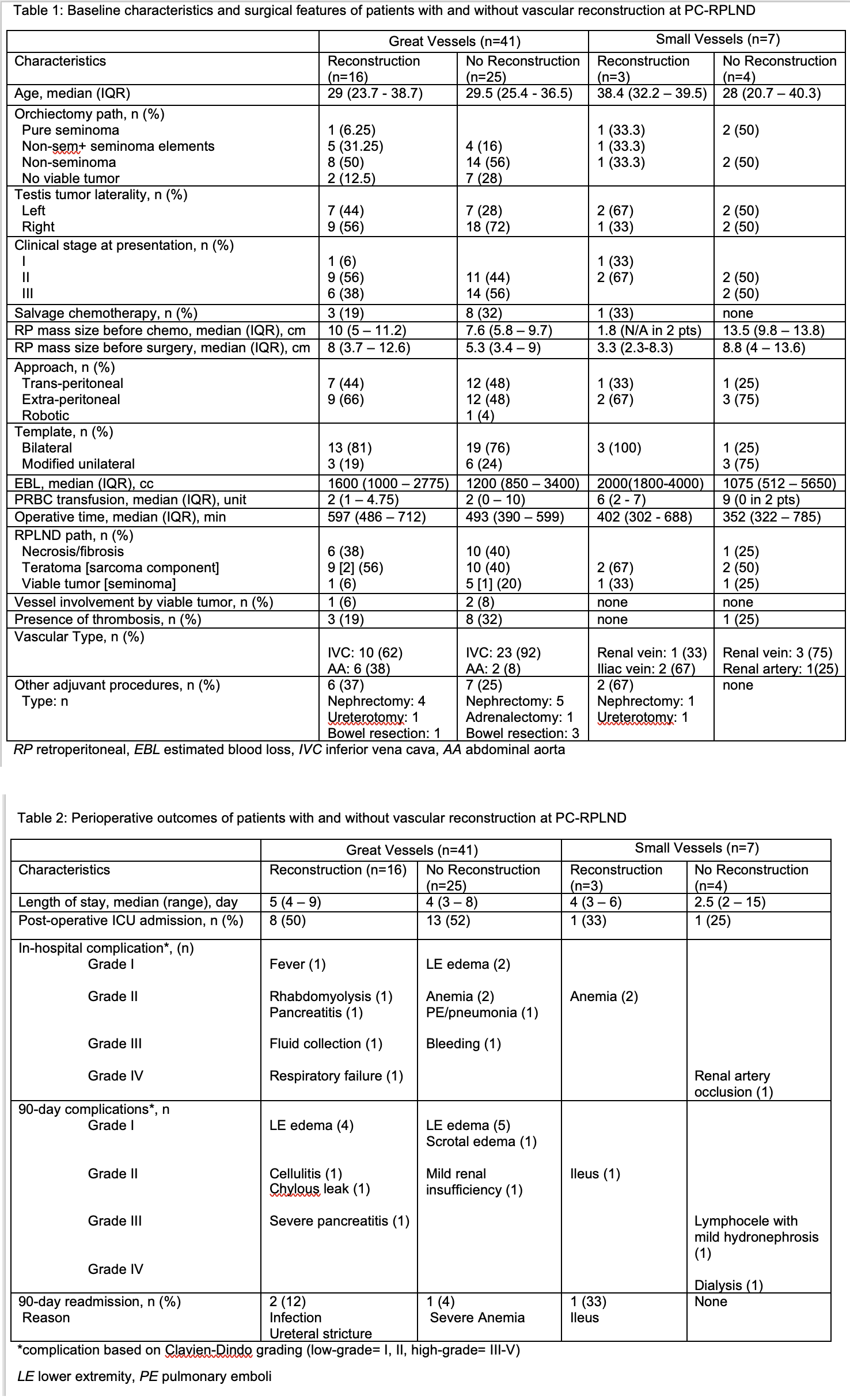
Results: A total of 1903 (ERAS=725 and non-ERAS=1178) patients were included in this study. The baseline and clinicopathological features of the patients are shown in Table-1. In multivariable analysis adjusting for other relevant factors, ERAS was not independently associated with recurrent-free and overall survival following RC (HR 0.87, p=0.3 and 0.84, p=0.19, respectively) (Figure-1).
Conclusions: Enhanced recovery after surgery protocols fails to impact the long-term oncologic outcomes in patients undergoing RC for bladder cancer.